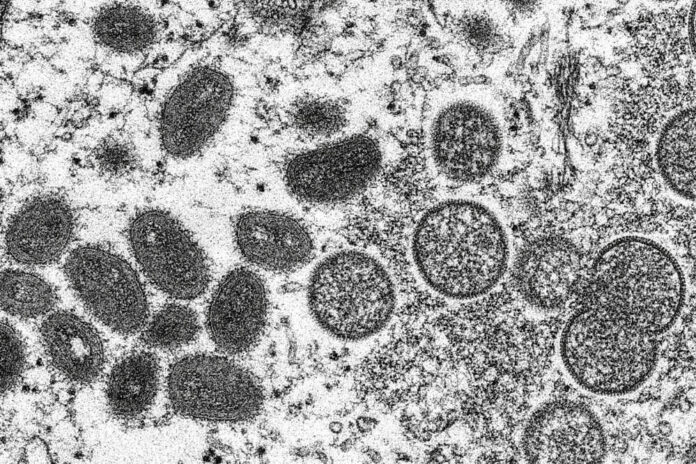
This 2003 electron microscope image made available by the Centers for Disease Control and Prevention shows mature, oval-shaped monkeypox virions, left, and spherical immature virions, right, obtained from a sample of human skin associated with the 2003 prairie dog outbreak.
Cynthia S. Goldsmith, Russell Regner | CDC via AP
Indiana health officials announced over the weekend that the first probable case of monkeypox in Indiana this year has been identified.
Indiana Department of Health could not release further information about the patient due to privacy concerns, officials said in a press release Sunday.
Initial testing of the monkeypox sample was completed at IDOH Laboratories Sunday and confirmatory testing is pending at the Centers for Disease Control and Prevention (CDC) laboratory. Based on the initial positive test and preliminary case investigation, state health officials consider this a probable monkeypox infection, state health officials say.
The patient remains isolated and officials are working to identify anyone the patient may have had close contact with while infectious, officials say.
“The risk of monkeypox among the general public continues to be extremely low,” State Health Commissioner Kris Box said in the release. “Monkeypox is rare and does not easily spread through brief casual contact. Please continue to take the same steps you do to protect against any infection, including washing your hands frequently and thoroughly, and check with a healthcare provider if you have any new signs or symptoms.”
According to the CDC, 113 monkeypox cases have been confirmed in 21 U.S. states and territories this year.
Earlier this month, the CDC discovered evidence that monkeypox may have been spreading in the U.S. earlier than was previously known. That’s because cases among patients without known contact with an infected person have been discovered. However, analysis from many more patients will be needed to determine how long monkeypox has been circulating in the U.S. and elsewhere, said Jennifer McQuiston of the Centers for Disease Control and Prevention.
“I think it’s certainly possible that there could have been monkeypox cases in the United States that went under the radar previously, but not to any great degree,” she told reporters June 3. However, she added, “there could be community level transmission that is happening” in parts of U.S. where the virus has not yet been identified.
It’s not clear how long infections have been happening, or where. CDC officials say some infections may have been misdiagnosed as something else.
Monkeypox is endemic in parts of Africa, where people have been infected through bites from rodents or small animals. It does not usually spread easily among people.
In May, cases began emerging in Europe and the United States. Many — but not all — of those who contracted the virus had traveled internationally, and health officials in a growing number of countries are investigating.
Hundreds of other cases have been found in other countries, many apparently tied to sexual activity at two recent raves in Europe. So far, many of the reported cases outside Africa have been in men who have sex with men, but health officials stress that anyone can get monkeypox. One heterosexual woman is among the U.S. cases under investigation, officials said.
No monkeypox deaths have been reported in the U.S. or Europe so far. But that could change if infections start occurring in more vulnerable people, like very young children or people with weakened immune systems, Dr. Angela Rasmussen, a virologist at the University of Saskatchewan told the Associated Press.
Even if outbreaks among people are contained, it’s possible the virus could take hold in the U.S. rodent population — either through pets or unwelcome rodents in homes, Rasmussen said.
Person-to-person transmission is possible either through contact with body fluids, monkeypox sores or contaminated items, such as bedding or clothing, or through exposure to respiratory droplets during prolonged face-to-face contact, state health officials say.
Monkeypox typically begins with fever, headache, chills, muscle aches and exhaustion about five to 21 days after exposure. Within one to three days — sometimes longer — after the appearance of fever, the patient develops a rash, often beginning on the face and then spreading to other parts of the body. Some people may only develop the rash, state health officials say.
The illness typically lasts for two to four weeks. People are considered infectious until all scabs from the rash have fallen off, state health officials say.
The Associated Press contributed to this report.




