
A private infusion room for patients receiving chemotherapy at Community Health Network MD Anderson Cancer Center-South, as seen in 2020.
Submitted photo
New diagnoses of six major types of cancer fell abruptly as the COVID-19 pandemic began to affect the U.S., a new federal report shows.
In a new report released last week, researchers with the National Cancer Institute detailed a drop in cancer screenings and subsequent diagnoses that occurred in early 2020 — during the early days of the COVID-19 pandemic. Researchers say the data triggered concerns about cancer outcomes in the coming years.
The federal report is not the first to look at the possible effects the pandemic had on cancer screenings. Research published in the Journal of the American College of Surgeons in May warned of a potential increase in undiagnosed cancer because of COVID-19 screening delays.
Decreasing rates
In the May study, researchers at Boston University developed a model to quantify missed diagnoses of lung, breast, and colorectal cancers by comparing observed cancer rates in 2020 with pre-pandemic cancer rates from the period of 2010-2019.
After analyzing data from 1,707,395 lung, 2,200,505 breast, and 1,066,138 colorectal cancer patients, researchers found significant differences between observed cancer rates — all decreases. Colorectal cancer decreased by 18.6%, lung cancer by 18.1% and breast cancer by 14.6%, the study shows.
While the incidence rates decreased, there is “no reason to believe” cancer incidence dropped during the pandemic in 2020, Dr. Kelsey S. Romatoski, a general surgery resident at Boston Medical Center and one of the study’s authors, said in a news release. It was more likely “reflective of missing cancer diagnoses,” she said.
The National Cancer Institute report, which is part 2 of their Annual Report to the Nation on the Status of Cancer, provides more evidence that there were declines in the number of diagnosed cases of cancers. While the Boston University Study looked at only colorectal, lung and breast cancers, federal researchers looked at three additional cancers: pancreas, prostate and thyroid cancers.
Researchers say the declines can be attributed to many people canceling or postponing cancer screenings while staying home during the pandemic, which can delay a diagnosis or care.
After analyzing cancer incidence data for 2015 to 2020 and comparing the number of newly diagnosed cases in 2020 with what was expected based on previous years, researchers found brief decreases in cancer diagnoses.
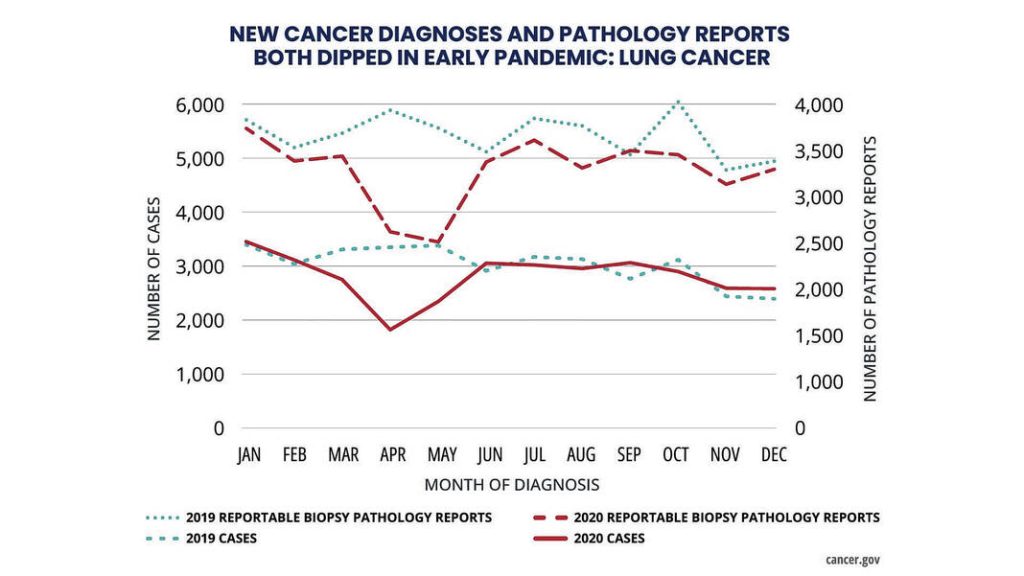
From March to May 2020, new cases of all six cancer types fell sharply. But by July 2020, diagnoses of all cancer types except prostate cancer had returned to pre-pandemic levels, with little difference between observed and expected numbers during the second half of the year, researchers said.
Breast, lung and colorectal cancers are often diagnosed through screening tests or other forms of early detection that may have been disrupted by the pandemic. Thyroid and prostate cancers are often diagnosed incidentally, while pancreatic cancer is usually diagnosed when the patient presents with symptoms, according to the report.
Data also showed the volume of pathology reports decreased during early 2020 as well. Pathology reports are used by medical providers to determine a diagnosis or treatment plan for specific conditions, such as cancer.
The findings suggest the decrease in new cancer diagnoses was not because of delays in reporting caused by the pandemic, but rather because of missed screenings and delays in other cancer-related procedures. Fewer in-person medical visits also likely contributed to the underdiagnoses, particularly for diseases such as thyroid cancer, which is often caught incidentally during other medical procedures, the report says.
Local effects
Doctors at area hospitals have seen the effect the COVID-19 pandemic had on screenings and diagnoses first-hand.

Dr. Sandeep Bhave, a board-certified radiation oncologist at Franciscan Health, said the pandemic “profoundly impacted” their regular screening and wellness checks, especially for colorectal and cervical cancer. Before the pandemic, people were undergoing colonoscopies and other screenings more routinely — allowing doctors to catch malignancies earlier.
After the pandemic, doctors have seen a phenomenon where they would catch malignancies later in diagnosis, Bhave said.
“More advanced rectal cancer, we saw very commonly, as well as more advanced cervical cancer,” he said. “We also screened for lung cancer and breast cancer as well, and saw similar things because patients felt reluctant to get screening tests during the pandemic.”
Doctors at Community Health Network have also seen an uptick in advanced cancers after the pandemic, particularly breast and colon cancers, said Dr. Pablo Bedano, a specialist in hematology and medical oncology.
Advanced cancers are cancers that may have been caught at an early stage if that patient had been screened, but are now in a stage where they cannot be eradicated by surgery, chemotherapy or radiation. Instead, doctors to treat them to try to keep them under control, Bedano said.
The increase in advanced cancers was mainly because of delays in diagnosis, as people were unable to get procedures or screening tests done, he said.
“In some cases, they missed one test and then they never fully scheduled for future testing, and so that led to later diagnosing now,” Bedano said. “I have to say that over the last year, things are catching up, and we’re getting back to our normal levels.”
Bedano recalled a recent instance where a woman was diagnosed with advanced breast cancer. The woman’s last mammogram was in 2019, and she didn’t have one in 2020 or in subsequent years.
“When she came to the hospital, she had a pretty large breast mass, and that was maybe six months ago,” he said.
Bhave said the pandemic particularly affected those who were on the cusp of beginning screenings. It also affected elderly patients in their late 60s and early 70s who were forced to miss regular screenings, he said.
Shutting down elective procedures in the early days of the pandemic “threw a wrench” into the system, Bedano said.
“It’s taken a long time to get people to accept screening,” he said. “And then if you pause it for a year, it takes a long time to get it back up and running. That has led to a lot of late cancer diagnoses.”

Now though, screening levels are getting back to normal at Community Health, Bedano said.
“Most of the screening programs are back up and running, and I think we’re getting back on track with early diagnosis,” he said.
Data from Community Health Network shows that since 2020 screenings have increased each year for mammograms and colonoscopies.
Mammogram screenings increased by 15.5% from 2020 to 2021, 10.9% from 2021 to 2022 and 7.8% from 2022 through August of this year. The 7.8% is based on August year-to-date annualized for a full year, a Community Health spokesperson said.
Colonoscopies increased by 35% from 2020 to 2021, 12.3% from 2021 to 2022 and 10.1% from 2022 through August of this year, annualized, data shows.
While the trend has improved, Bhave says overall screening is lower than it was pre-pandemic at Franciscan. A rise of medical distrust may be a factor in this, he said.
“As a consequence, there has been maybe a lower effort for some patients to get screening,” Bhave said.
At the beginning of the pandemic, people didn’t want to come to the hospital and have procedures. Additionally, the nature of the pandemic and the changing recommendations for it created distrust in the medical field, Bedano said.
“First, no masks and then masks, and when do you get the vaccine? I think that created some distrust,” he said. “But again, I think things are getting back to normal now. That’s my feeling.”
Screenings are vital
Statewide cancer screening rates from 2020 show that Indiana tends to have higher rates of screenings.
Nearly 78% of women ages 21-65 reported having a pap screening for cervical cancer during the previous three years, and nearly 74% of women ages 50-74 reported having a mammogram screening for breast cancer in the previous two years, according to a 2021 report from the Indiana Cancer Consortium.
A little more than 71% of adults ages 50-74 had met colorectal cancer screening recommendations. However, only about 29% of men over the age of 40 reported having a prostate-specific antigen, or PSA, test in the previous two years, according to the report.
Bhave says it’s on doctors to encourage patients to get routine screenings because it can help catch cancer earlier, and in some cases, prevent cancer from happening and save lives. This is especially true for colonoscopies, he said.
Colonoscopies tend to save more lives compared to other procedures because most colon cancers start off as a polyp, or a projecting growth of tissue from a surface in the body. It takes about three years for it to turn into cancer, giving people a window of time to catch it, Bedano said.
“If you catch it in the polyp stage, or the early cancer stage, you can make a big difference,” he said.
There’s been such an increase in these cancers happening in younger people that guidelines for colonoscopies were changed. Now the recommendation is to start screening at 45, instead of 50, for colon cancers, Bedano said.
For breast cancers, screenings are recommended starting at 40 for women. For prostate cancer, although it’s not mandated at age 45, men can start talking about having a PSA test at that age. Smokers who are 55 and older should get a CT scan every year for lung cancer, Bedano said.
A lot of the fear in doing a cancer screening is because of the unknown. At the same time, it’s a really important, Bhave said.
It’s also generally covered by most insurance providers and is heavily advocated for by primary care doctors.
“I would encourage them to see their primary care doctor this year to see where they are with their screening, and whether they … need to get screening tests done,” Bhave said.




