The diagnosis changed his world, even though he knew it would one day come.
More than one doctor had told Greenwood resident Greg Hill that “every man is going to get prostate cancer if he lives long enough.” The 73-year-old knew “his number” would be up sooner than later; after all, his father had died from the disease.
But still, Hill figured he’d be closer to 80 years old when the diagnosis was made. He found out he had prostate cancer in 2018 at the age of 67 — nearly 13 years sooner than he ever would’ve thought.
“There’s a million thoughts that go through your head, wondering what’s going to happen,” Hill recalled.
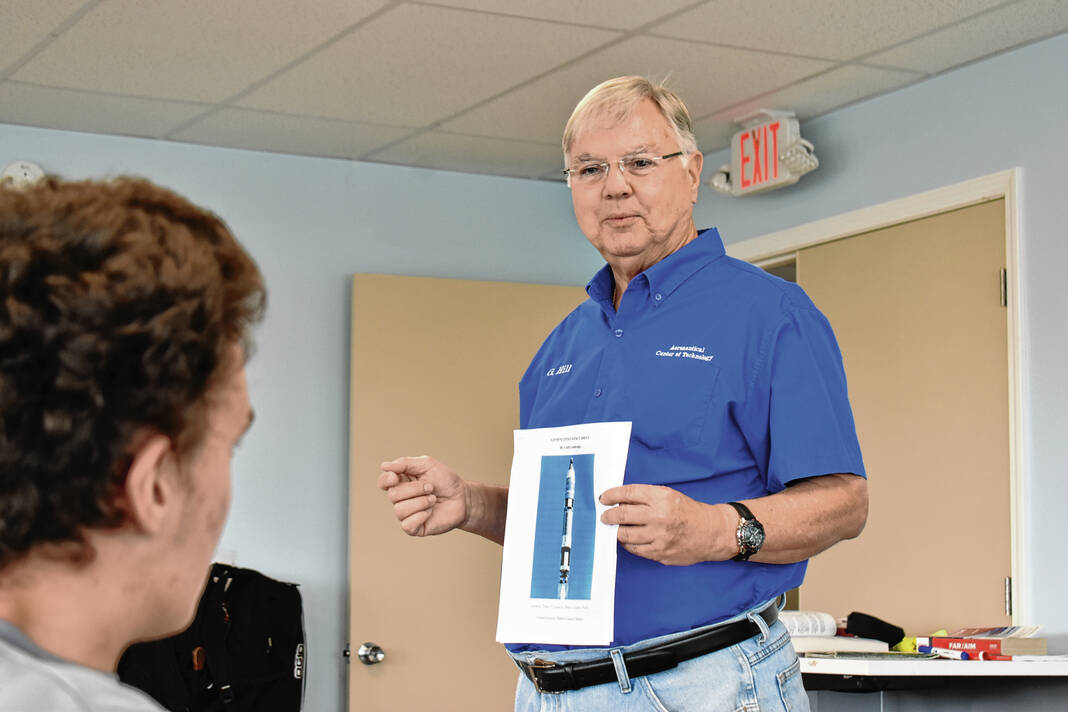
Hill is a licensed pilot and an instructor at the Aeronautical Center for Technology at Indy South Greenwood Airport. The Purdue engineering graduate is a member of the Greenwood Economic Development Commission, and has been the chapter president of the local Experimental Aircraft Association chapter, No. 1354, for the past five years.
Something was off
For the last several years, Hill has had his doctor check his prostate-specific antigen, or PSA, level. Prostate-specific antigen is a protein made by the prostate, a walnut-shaped gland that’s part of the male reproductive system. PSA levels can be measured in the bloodstream, with elevated levels sometimes being a sign of prostate cancer. Levels for men who are 60 and older should be at or below 4 milligrams per milliliter and 59 and younger should be at or below 2.5, with the average PSA for the younger group being less than 1 milligram per milliliter, according to the MD Anderson Cancer Center.
But about six years ago, Hill’s primary care doctor noticed something was off with his PSA. It had slowly been creeping up, which is to be expected as he got older. His PSA eventually got up to nine, which was a concern of his doctors.
A year later, Hill had his PSA checked again. It had jumped to 25 milligrams per milliliter in less than two years — a very concerning development. Anything above 21 is considered a high elevation, according to the MD Anderson Cancer Center.
“Now this set off alarm bells in the doctor’s office,” Hill said.
His primary care physician helped him set up an appointment with Urology of Indiana, which is coincidentally next to the Greenwood airport. That test showed his PSA topping out — another red flag, Hill said.
Hill then went in for a biopsy, as sometimes there can be false positives and negatives. They took 17 “core samples” of his prostate, and nine of the 17 — or a little more than half — came back cancerous.
Doctors had him undergo a scan to see if it had spread away from his prostate. If it had spread to his hip joints, for example, he wouldn’t need treatment because it would be too late for it, he said.
It hadn’t yet, which meant there was time to do something about it. His Gleason Score, a way to measure the aggressiveness of prostate cancer and help determine treatment option, was 4 + 3, which is at the high-end of the medium-grade group for the cancer, he said.
A lower grade usually indicates a better chance of successful treatment, while a higher grade group means the cancer is more likely to spread aggressively, according to the American Cancer Society.
While his doctor, Jason Sprunger, said his score wasn’t “terribly bad,” it was a serious concern, Hill said.
He had a decision to make about whether the prostate gland and its internal tumor should be removed.
“I think [Sprunger] thought that he was going to have an uphill battle with me to do something about this,” Hill said. “Instead, I said, ‘Take the worthless damn thing out.’ Just like that.”
So, Hill had the operation to have his prostate gland and tumor removed, going to Franciscan Health for the operation. Removing the tumor was a 3.5-hour operation, with the equipment to do so only available on certain days. His daughter came up from Texas to take care of him during this time, and he spent two nights in the hospital waiting for his body to “return to normal” after the surgery and the anesthesia, he said.
Not completely gone
Post-surgery, Hill underwent follow-up PSA tests. Pathology reports showed the cancer had not spread beyond the prostate capsule, to his lymph nodes.
However, his PSA level was stuck at 0.4 milligrams per milliliter instead of zero. Over the next six months, the level would slowly increase by a tenth of a point each time he had a test, Hill said.
“[Doctors] said, ‘Well, there has to be some stray cancer cells in there,’” Hill said.
Hill’s doctors recommended he consider external beam radiation therapy. This type of treatment uses a proton beam to “zap” cancer cells.
Over the course of two months, he was “zapped” 39 times by a machine, named “Bessie.” The treatment itself was “painless,” but there were one or two unpleasant side effects, which subsided in a few weeks. His PSA went back down to 0.1, he said.
Hill was thrilled.
“OK, I’m finally done dealing with this,” Hill said.
He still went in for follow-ups to monitor his PSA over the course of the next year. Then in June 2023, it was discovered his PSA had again gone up, with a test showing it being at 3.6 milligrams per milliliter.
Doctors were again concerned. They scheduled Hill for a PET scan, he said.
For the scan, they gave Hill an IV injection containing some “radioactive sugar water,” which is used to “light up” organs as they absorb the water, he said. It will also show any lymph nodes that have cancer cells, as they’ll light up too.
The scan revealed that Hill had three lymph nodes in his abdomen that had cancer cells in them.
Hill suggested to Dr. James Raybourn, his new doctor at Urology of Indiana as his old doctor had retired, that they use liquid nitrogen to kill the cancer. But this presented a problem.
“He goes, ‘Well, the problem with that is we kill those three and then three more pop up somewhere else, and it’s like whack a mole,” Hill said.
Raybourn suggested Hill undergo hormone replacement therapy, or HRT, using injections of Lupron. Prostate cancer cells feed on testosterone, which is produced by males, so if the production of testosterone is stopped, the cancer cells are starved and die, Hill said.
But Hill was hesitant about the treatment. He had researched the treatment online and had read reviews from men all over the world about it, with some reviews discussing some alleged unfortunate side effects, he said.
“I thought, ‘You know what, I don’t think I like that idea and I wasn’t going to do it,’” Hill said.
Another way to treat it

Two conversations helped change Hill’s perspectives on the treatment.
A friend at the airport, a physician’s assistant, told Hill that when clinical studies take place for a drug, any side effect has to be reported. He also talked to a cousin of his about the situation, discovering that not only did that cousin have prostate cancer six years earlier but that he had it removed and underwent the same treatment.
“He said, ‘I have been on Lupron for six years.’ And he said, ‘It’s not as bad as you think,’” Hill said. “I said, ‘OK, I’ll do it.’”
After speaking with his daughters, he told his doctor he wanted to take Lupron. Since then, he has taken a shot every three months or so, going back in to have his PSA checked, he said.
“With one injection of Lupron, my PSA went from 3.6 [milligrams per milliliter] to less than 0.01 — undetectable, which is what they were hoping for,” Hill said.
Hill has now gone through a year’s worth of Lupron shots with the same undetectable result.
In June of this year, one year after the PET scan that showed cancer in his lymph nodes, Hill learned exactly how many cancer cells he had. The cancer cells were a “pinpoint of light” on the scan and would not have been able to be seen on a regular CT scan or MRI, Hill said.
After a discussion with his doctor, Hill had a follow-up PET scan scheduled which took place this past August. A few days after this, he got a report from the radiologist.
“It said, ‘Patient was scanned from base of skull to mid-thigh. No abnormal activity was observed,’” Hill said.
It was the news Hill and his doctor were waiting for.
“I’m happy now that I’ve got another 20 good years left, because I’ve still got a lot that I want to do,” he said.
On that list: continuing to teach students at the Aeronautical Center, where he teaches a rocketry class and beginning computer programming, and taking part in the Young Eagles, an EAA program, and the Airport Day held at the airport every year.
“I’ve been flying for 47 years, and I’ve been giving people airplane rides ever since I got my license, starting with my grandmother,” Hill said. “I enjoy doing that, so I’m not ready to just roll over and die right now. I’m ready to get out here and keep going strong with it.”
Hill is going to continue to take Lupron for another year, just to make sure everything is OK. After this, Hill’s doctor gave him permission to go off the medication for a while, and doctors will continue to monitor his condition to see if any problems come up. If any do, he’ll go on the drug again, he said.
Checking PSAs
Looking back, Hill said it took him some time to process the cancer diagnosis.
“You always think, ‘This can’t happen to me. It happens to somebody else.’ But it does happen to you, and it takes a while to process that information,” he said.
It is a “little bit scary” not knowing if he is going to win the battle against cancer. He thought often about his stepmother, who did everything doctors wanted but still succumbed to breast cancer. He didn’t want to go through a similar experience, he said.
He also initially questioned whether he really had cancer, as he felt “healthy as a horse.” But people can’t necessarily feel whether they have it, he said.
Hill originally kept his cancer diagnosis relatively secret, only telling his family and those close to him — though he did ask them not to tell his mother before he found out if he had optimistic news. He eventually went public in a Facebook post on his personal page about his experience, about a year-and-a-half after he was diagnosed, he said.
He received a lot of support from his family and friends, with many saying they were praying for him, he said.
With the Lupron treatment going well, he is feeling optimistic about his future. Hill also hopes his story will encourage other men to get their PSA level checked —regardless of age.
“This is a way for my story to reach men that I don’t know, and hopefully inspire them to go see their doctor, get their PSA checked. Do something about it before it’s too late,” Hill said.
Hill also wants to offer himself as a resource to anyone who may be going through a similar experience with prostate cancer, or who just wants to ask him questions or for advice. He can be reached via email at [email protected].
THE HILL FILE
Name: Greg Hill
Age: 73
Diagnosis: Prostate cancer
Treatment: Tumor removal, followed by external beam radiation therapy and Lupron hormone replacement therapy
What has cancer taught you?
“What it has taught me is that modern medicine has solutions for these problems — you don’t have to just roll over and die. … Fight the battle, do what your doctor wants you to do, go through the procedures — do everything that they tell you to do, and hope for the best. … It’s also taught me that I want to make other men aware and hopefully inspire them to to get themselves checked out.”
How has cancer changed you?
“It forces you to face your own mortality down the road. It also tells you to make the best of whatever time that you have left. I am still going to do everything I can at the tech center. My classes, I’m going to be doing that for as long as I can get out of bed and remember my name in the morning. I’m still going to be flying kids as long as I can, and everything else out the airport that I’ve been doing for years and years. The other thing is you can get into a sometimes dull and boring routine in your life, and I have decided that for the next 20 years, I’m going to do everything I can to enjoy life.”
What would you tell someone just diagnosed?
“I guess I would ask him, ‘Do you want to hear what I went through in a nutshell so you will have an understanding, a preview, if you want to call it that, of what is in store for you?’ … I’m not one to ask a person a bunch of nosy questions, but if someone asks me for advice or my opinion, I’ll give it to them straight: Here’s what you’re faced with, here’s what I went through, and in all likelihood, you are going to follow those same steps. Hopefully, when you get done, you are going to find that you’ve still got a long life ahead of you.”