Indiana’s coronavirus cases surged by more than 300 to nearly 1,000 statewide Friday, as seven more deaths were reported, bringing the state’s death toll to 24 amid the pandemic, state health officials said.
Johnson County’s numbers seemed to hold steady Friday with just two new cases after a local surge on Thursday, according to the Indiana State Department of Health. But local health and public safety officials suspect the number of local cases is much higher than what the state is reporting, and were working Friday to nail down a number, said Mike Pruitt, spokesperson for the county’s incident management team.
“Test results are coming back in bulk now,” Pruitt said.
The local death toll has not changed. Three Greenwood residents, all over the age of 75, have died from the virus.
At Otterbein Franklin SeniorLife Community on Friday, officials were still waiting on the results of eight additional COVID-19 tests that were given Thursday, and weren’t expecting them until Friday night, possibly Saturday. Those eight residents are being treated as if they have COVID-19, said Gary Horning, spokesperson for the Franklin senior care facility where an outbreak was reported this week.
Seven residents were transferred to area hospitals late Wednesday night after testing positive for the virus. Plans were in the works Friday to transfer three of them home or back to Otterbein, where they will be in isolation. Four will remain hospitalized, Horning said.
The outbreak originated with a therapist who was admitted to the hospital and tested positive. A nurse has also contracted the virus, Otterbein officials said.
Otterbein Franklin has more than 500 residents, 165 of whom are in the nursing home where the outbreak has occurred, and about 300 employees, Horning said.
Local officials know there is a second outbreak at a separate senior care facility in Johnson County, but they do not know which one, Pruitt said. Otterbein reported its outbreak to authorities, which is how they found out about it, he said.
The county’s hospital was better prepared Friday for another surge.
Johnson Memorial Hospital on Friday opened a COVID-19 unit. The new unit is part of a $47 million expansion the hospital began construction on more than two years ago. The new emergency and outpatient services department will instead make its debut as an isolation wing for COVID-19 patients.
The unit is completely separate from the hospital and has 24 beds, with room to add four more if necessary, said Dr. David Dunkle, president and CEO of Johnson Memorial Health.
On Friday, the Franklin hospital had four confirmed COVID-19 patients, and was awaiting test results for eight others.
“It’s a game-changer for us to be able to isolate these patients from the rest of the hospital,” Dunkle said. “That makes other people feel better, too — to know that we’re keeping those COVID (and) COVID-potential patients on a different side of the hospital.”
The new unit’s air supply is also completely separate from the rest of the hospital, which helps keep the extremely contagious virus more isolated, Dunkle said.
“Our engineers were able to turn some of the trauma rooms into negative air spaces,” he said. “We’re able to vent that air out so it doesn’t spread throughout the rest of the hospital.”
Hospital staff felt a sense of relief Friday, Dunkle said.
“I could definitely sense an uptick in people’s moods today, which was nice,” he said.
Staffing the unit will be a challenge as far as reworking schedules goes, Dunkle said. At the moment, eight of the symptomatic patients are on the same floor, so staff can be condensed to that one area to be more efficient, he said.
“We’re trying to stay as efficient as possible as far as staffing goes,” Dunkle said.
If the COVID-19 unit fills, the hospital has three isolation rooms in other parts of the building they can also use. Patients can also be placed in private rooms with the door closed. But that is not ideal because those rooms are not designed to be used for isolation purposes, Dunkle said.
“It is deemed safe for COVID-19 patients to be cared for in a regular room with the door closed,” he said. “Though that is not ideal, it is something hospitals will have to do.”
Indiana’s number of confirmed cases of COVID-19, the disease caused by the virus, grew by 338 to 981 across the state, the Indiana State Department of Health said.
Nearly 7,000 people statewide have been tested for the coronavirus, department officials said Friday, citing test results reported to the state agency, which also released its first demographic data on Indiana’s confirmed coronavirus cases.
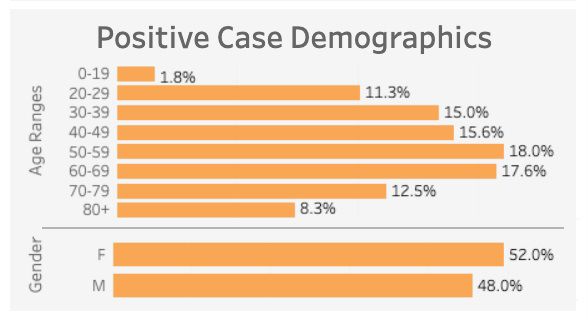
That data shows that slightly more females than males have been infected with the virus: 52% of the cases are women. About 56% of infections are among people aged 50 and older, and about 38% are among people age 60 and older — the age group most at risk of having a severe infection.
State health officials have said they are targeting tests for those most at risk and health care workers.
Coronavirus causes mild or moderate symptoms, such as fever and cough that clear up in two to three weeks. For some, especially older adults and people with existing health problems, it can cause more severe illness, including pneumonia, or death.
The data includes no information about how many of Indiana’s health care workers have been infected by the coronavirus.
Indianapolis accounted for 192 of the state’s 338 new cases, the state health department said Friday, and hospitals in the city are filling up fast.
As major metropolitan centers run out of space, hospitals such as Johnson Memorial in adjacent counties, will most likely fill up fast too, Dunkle said.
If the pandemic reaches that point, all hospitals across the state will need to communicate to determine which can take patients, and the state health department has taken a lead on coordinating that communication, he said.
“You’ll hear stories about beds being put in hallways, or patients being put in units not made for isolation,” Dunkle said. “What we really need to do across the state of Indiana is communicate who has open beds, who has ventilators.”
State health officials, so far, have not been willing to share that information.
Johnson Memorial has 13 ventilators total, and none of its current COVID-19 patients are using them, Dunkle said.
The Associated Press contributed to this report.





